Caregivers of HIV-positive
children were interviewed in the Mbarara and Isingiro districts of Uganda to
identify current trends in practices related to HIV testing and the disclosure
of HIV status to the child.
A total of 28 caregivers of at least one HIV-positive child participated in semi-structured interviews exploring when and why they tested the child for HIV, when the child was informed of their positive status, and what the caregiver did to prepare themselves and the child for status disclosure.
For a majority (96%) of respondents, the decision to test the child for HIV was due to existing illness in either the child or a relative. Other common themes identified included the existence of stigma in the caregivers’ communities and doubt that the children truly understood what was being explained to them when their status was disclosed. Most (65%) children were informed of their HIV status between the ages of 5 and 9, with the mean age of disclosure occurring at the age of 7. General provision of HIV information typically began at the same age as disclosure, and as many as two thirds (64%) of the caregivers sought advice from an HIV counsellor prior to disclosure. How a caregiver chose to prepare themselves and the child did not affect the caregiver’s perception of whether the disclosure experience was beneficial or not.
These findings suggest that the HIV disclosure experience in Mbarara and Isingiro districts differs from current guidelines, especially with respect to age of disclosure, how caregivers prepare themselves and the child, and approaching disclosure as an ongoing process. The doubts expressed by caregivers regarding the child’s level of HIV understanding following the disclosure experience suggest the children may be insufficiently prepared at the time of the initial disclosure event.
The findings also suggest that examining the content of pre-disclosure counselling and HIV education, and how health care professionals are trained to facilitate the disclosure process as important avenues for further research.
A total of 28 caregivers of at least one HIV-positive child participated in semi-structured interviews exploring when and why they tested the child for HIV, when the child was informed of their positive status, and what the caregiver did to prepare themselves and the child for status disclosure.
For a majority (96%) of respondents, the decision to test the child for HIV was due to existing illness in either the child or a relative. Other common themes identified included the existence of stigma in the caregivers’ communities and doubt that the children truly understood what was being explained to them when their status was disclosed. Most (65%) children were informed of their HIV status between the ages of 5 and 9, with the mean age of disclosure occurring at the age of 7. General provision of HIV information typically began at the same age as disclosure, and as many as two thirds (64%) of the caregivers sought advice from an HIV counsellor prior to disclosure. How a caregiver chose to prepare themselves and the child did not affect the caregiver’s perception of whether the disclosure experience was beneficial or not.
These findings suggest that the HIV disclosure experience in Mbarara and Isingiro districts differs from current guidelines, especially with respect to age of disclosure, how caregivers prepare themselves and the child, and approaching disclosure as an ongoing process. The doubts expressed by caregivers regarding the child’s level of HIV understanding following the disclosure experience suggest the children may be insufficiently prepared at the time of the initial disclosure event.
The findings also suggest that examining the content of pre-disclosure counselling and HIV education, and how health care professionals are trained to facilitate the disclosure process as important avenues for further research.
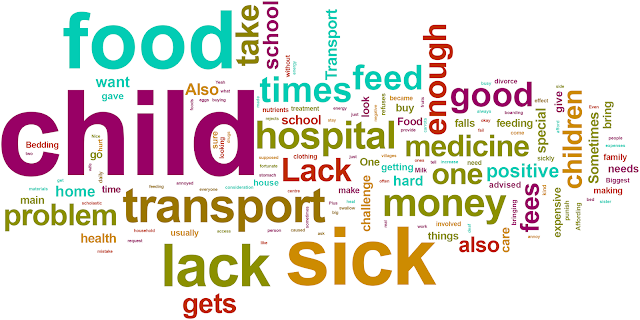
Below: Word Cloud
Below: General Attitude to Disclosure
Full article at: http://goo.gl/6s7Idb
By:
College of Pharmacy and Nutrition, University of
Saskatchewan, Saskatoon, Saskatchewan, Canada
Claire Card
Ministry of Health, Kampala, Uganda
Eisha Grant
Faculty of Medicine, Mbarara University of Science and
Technology (MUST), Mbarara, Uganda
Winnie Muyindike, Samuel Maling
Western College of Veterinary Medicine, University of
Saskatchewan, Saskatoon, Saskatchewan, Canada
More at: https://twitter.com/hiv insight


No comments:
Post a Comment